Dundee is known as the overdose capital of Europe, with twice the national average of overdose deaths and a high prevalence of hepatitis C. Community pharmacies – already in regular contact with people on Opioid Agonist Therapy (OAT) – were the cornerstone of this model of HCV care, which is helping move the city towards elimination.
Located on the River Tay is Scotland’s third largest city, Dundee. Dundee was once well known for its whaling and jute industries during the British empire however in the wake of World War Two, the city faced a major economic decline. While today Dundee has pockets of regeneration, according to the 2020 Scottish Index of Multiple Deprivation Dundee City has one of the highest levels of deprivation in the country.
While heroin has historically been the injecting drug of choice, over the past decade the increase in cocaine, crack cocaine and benzodiazepines has altered the drug use landscape. Dundee has twice the national average of drug-related deaths which has earned the city the unwanted moniker of overdose capital of Europe.
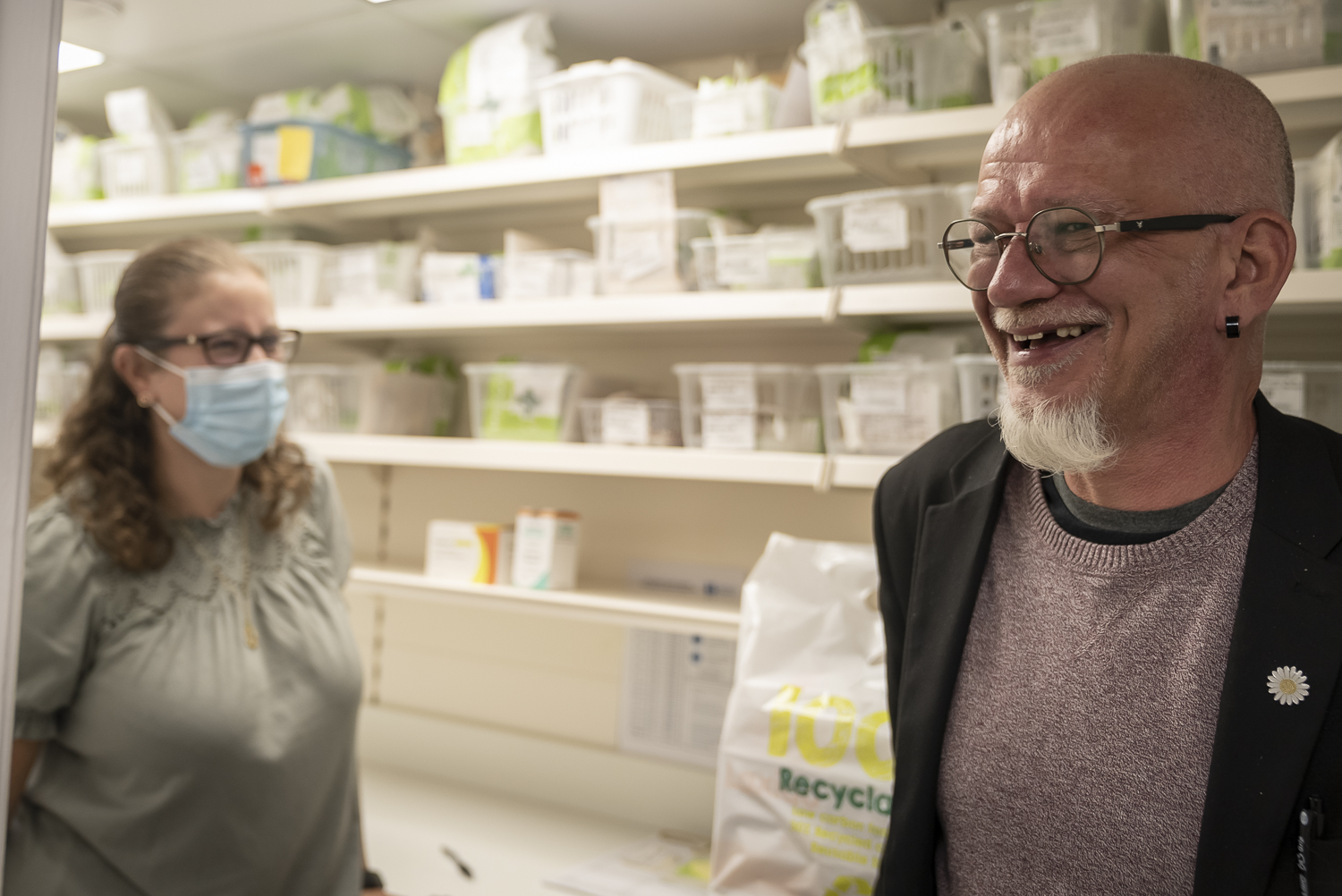
The Cairns Centre in Dundee is well known and trusted service among many of the city’s 4,500 drug users. Operated by third sector organisation Hillcrest Future, the Cairns Centre is one of two primary needle & syringe exchange sites across Tayside. While sterile injecting equipment is also available from most pharmacies throughout the city, it is the relationships with staff and other services offered that have led to enduring connections with community members.


The role of needle and syringe programs
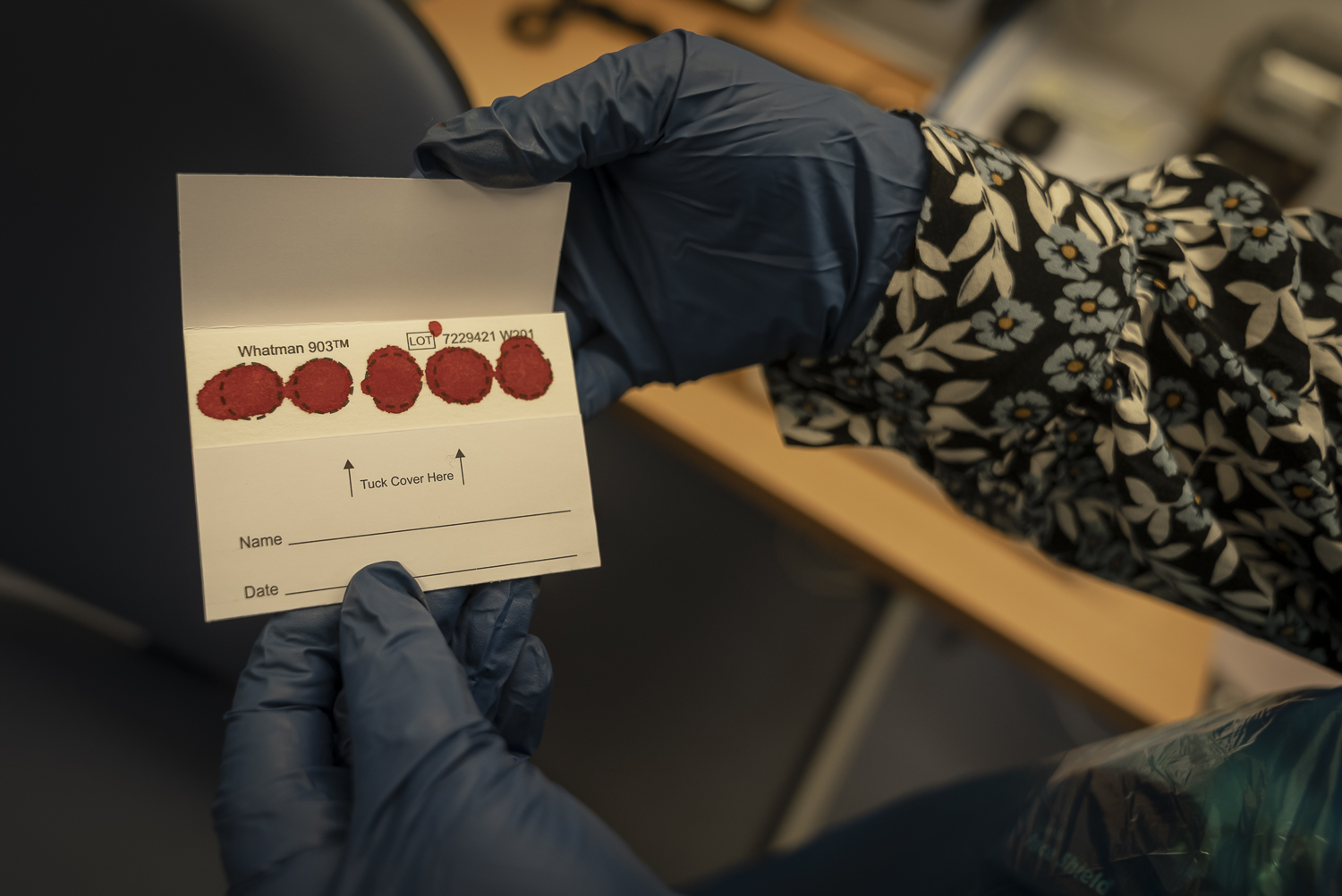
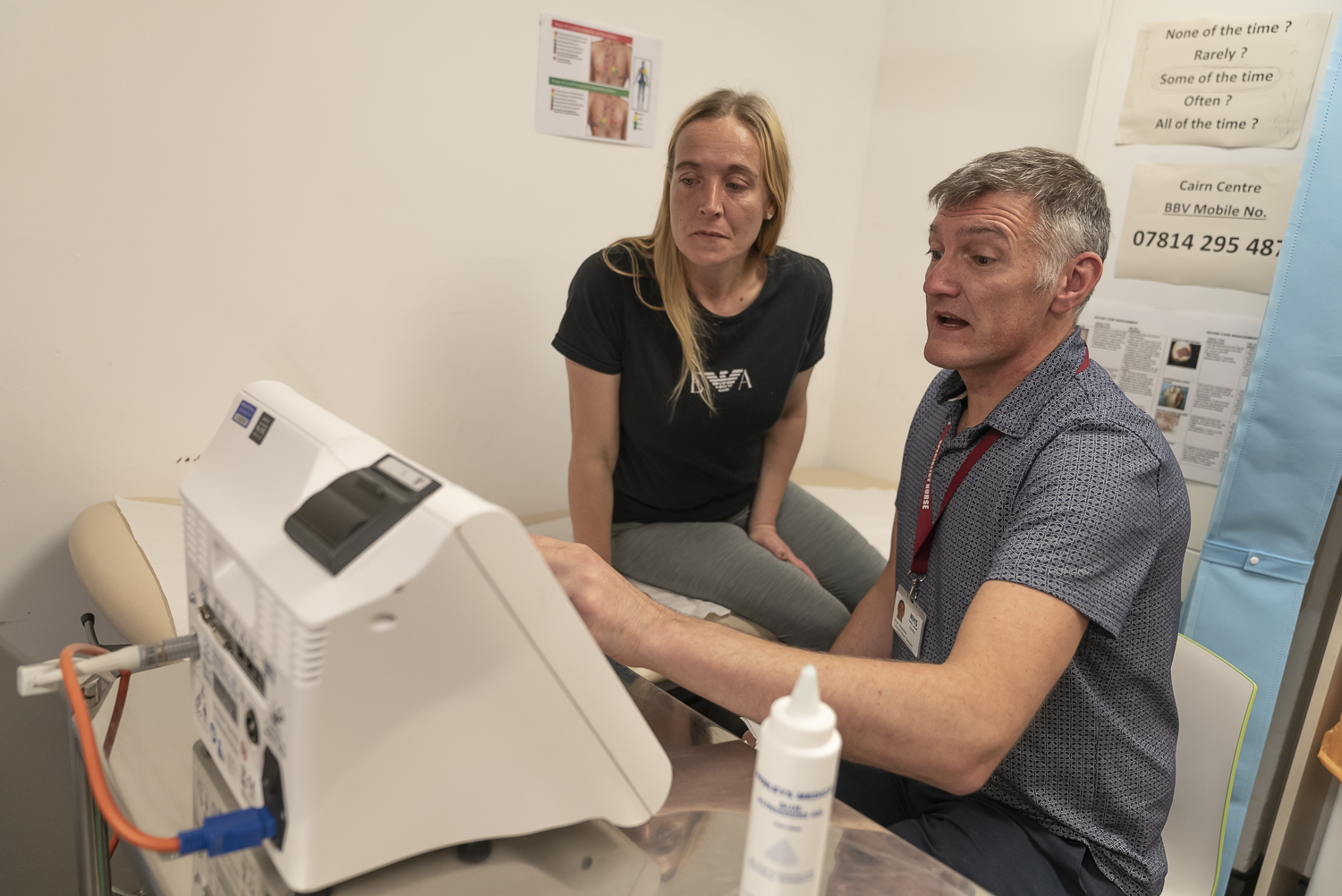
In 2009, the Scottish NHS (National Health Service) decided to build on the strong relationships between the Cairns Centre and embedded nurse Brian Stephens on site and also roll out DBS testing as the first method of mass testing.
“When I first joined the team in 2009 it was to make sure that I was embedded within services that had the best access to people who use drugs. Because as healthcare workers people who use drugs can often feel disenfranchised from healthcare, they might not have the best relationship with a general practitioner or other services and might have a low understanding of the issues around substance misuse. So I base myself on the needle exchange to make sure that I could have the relationship that was already well established with the workers who run this service. I could piggyback on the back of their relationship with the service users who I wanted to engage with.”
In 2009, 80% of people who accessed the service for sterile injecting equipment had never had a blood test before doing a DBS (dried blood spot) test at the Cairns Centre. At the time 94% of people came back with positive tests suggesting an incredibly high hepatitis C positivity rate. Unfortunately, the interferon-based treatments available at the time had major side effects and offered a low cure rate which meant that only a few people were prepared to undergo the treatment, let alone those who were successfully cured.
The new DAA treatments changed everything
When the new DAA (Direct Acting Antiviral) treatments entered the market in 2015, Prof John Dillon from the University of Dundee knew there was an opportunity to make major gains in testing and treating hepatitis C in the area.
“The key change was the arrival of the DAA and that allowed us all the rest of the parts of the jigsaw puzzle to fall into place. We could then really effectively treat everybody relatively easily. And so that took away the last of the blocks and barricades.”
The strength of the long-term relationships with the community and their earlier familiarity with testing for hepatitis C ensured that when the new treatments were available Brian and the NHS nursing team along with Hillcrest Future colleagues at the Cairns Centre began ramping up hepatitis C testing and treatment. In 2016 nurse practitioner Brian Stephens became accredited which further enhanced the team’s ability to quickly test and treat Cairns Centre clients.
“It was 2015 that I came in and did a dry blood test and that came back positive. When I got my test back it was a shock but I was relieved that we could do something about it, and when I started 2015 I was on the first tablet form. Well, positives came out of it and I was glad there was a cure for it.”

Immediate reach for communtiy pharmacies
For many community members that were successfully treated for hepatitis C at the Cairns Centre, it was their first positive experience with health care. This experience prompted Brian and the team to start engaging clients in broader aspects of their health. Today it is common for a nurse to provide a check-up that includes cardio tests, ECG and blood tests every six months to provide more holistic care for the ageing population.
The second central part of the hepatitis C elimination strategy was testing and treatment throughout the Tayside pharmacy network.
“Even a small pharmacy in Tayside would have a footfall of at least 1500 different people a week. The pharmacies reach well into the communities and we worked out 97% of our population would use a pharmacy at least once a year.”
Andrew Radley and Professor John Dillon began a data linkage project connecting the prescription records of people prescribed OST with the lab records of people that had been tested for hepatitis C. This data linkage project provided a framework for pharmacies to join the elimination effort and took on the challenge of testing all OST (Opioid Substitution Treatment) clients with a DBS test for hepatitis C at least once a year. The pharmacy pathway was crucial in testing and treating a population who are not necessarily active drug users and may not have or engage with a primary health care practitioner regarding their opioid dependency.
DBS testing meant fast and easy linkage to care
In the small town of Forfar, the Davidsons pharmacy is a hive of activity. Pharmacist Lauren Clarke and her team are always on the move filling scripts and attending to their client’s many needs.
“We were asked as a pharmacy to do the dry blood spot tests for Hep C. We had a list of all of our patients that we wanted to be tested every year. We would get their permission to check their medical records to see when they’d last been tested and if it was over a year then we would do it. Once we found out somebody’s positive and they’ve had their blood tested and we’ve requested a prescription it’s usually to us within a week and we can get the medication started as soon as it comes in.”
Community members Pamela and Scott are regulars at Lauren’s pharmacy and both have been treated for hepatitis C in the past year. Lauren or her assistant Jan often ask their clients while they’re picking up their methadone if they have time for a quick 5-minute DBS test This was how Scott’s second infection was picked up.

“I didn’t have to go to the hospital. My treatment was all done through the pharmacy, none of it was through the hospital the tests through to the treatment, to the results everything. It was all really good. We just pick up the tablets daily every day for 12 weeks when I would come in for my methadone and then you get Sundays takeaway.”
The pharmacy pathway across the Tayside region continues to provide highly successful in testing and treating significant numbers of people for hepatitis C. Similar to the approach at the Cairns Centre, the pharmacy model also builds on the strength of existing relationships and the ease and speed of a DBS test. Across the Tayside region, the IEP (Injecting equipment provision) pathway such as the Cairns Centre accounts for 28.8% of all successful hepatitis C treatment with community pharmacies responsible for the second largest amount at 20%.
The hepatitis C elimination story in Tayside is a major success. However, the work of maintaining elimination and focusing on the broader health needs of people who inject drugs is the next chapter in the Tayside story. According to Profession John Dillon “people who inject drugs do have a substantially reduced life expectancy, both from increased cardiovascular and respiratory disease but from drug-related death and how we break that cycle down, how we make injecting as safe as possible for those that choose to continue to do so is a key point. So that’s the next frontier that we need to be thinking about. And the teams that we’ve developed to deliver hepatitis C elimination are uniquely placed to move forward and to tackle those challenges.”